Do you know what happens when an athletic trainer, dietician, two social workers and a nurse get together to plan a simulation?
It started with Natalie A. Kružliaková, in the Department of Nutrition and Health Science, working with Dr. Judy Gray, and Kim Taylor in the Department of Social Work to come up with a patient scenario that incorporated elements to hit on themes for both Dietetics and Social work disciplines. We also worked with Dani Ely in Nursing’s Simulation, Information, and Technology Center, to ensure the scenario worked with the available technology in the sim labs, and welcome home suite.
Their collective efforts brought Yvette Washington, a 70 year old female, to life for their students.
Here’s an excerpt of her story from the case, “Yvette Washington was transported to Ball Memorial Hospital ED with right-sided hemiparesis and slurred speech. Confirmed lacunar ischemic stroke—NIH Stroke Scale Score of 12. Mrs. Washington was then admitted to the neuro acute care unit, and for the past five days has been receiving PT, OT, speech, and nursing services. MBSS completed; SLP recommended modified diet. RDN consulted to provide dietary recommendations post d/c.”
Once the basic parameters were set with the case background, Dr. Justin Tobyas, Director of Interprofessional Education and Practice, started gathering all the details to set the scenes. It took two weeks for him to gather empty snack wrappers for the home setting, as well as he asked for clean fast-food bags, pizza boxes etc. He then stained the food wrappers with mineral oil to give them authentic grease stains, but without the smelling like garbage. He even came up with a broken refrigerator by creating a thermometer prop for the fridge in the Welcome Home Suite. This simulation was created with $0 additional dollars out of the IPE budget, utilizing the simulation technology already invested in by the College of Health, and the School of Nursing.
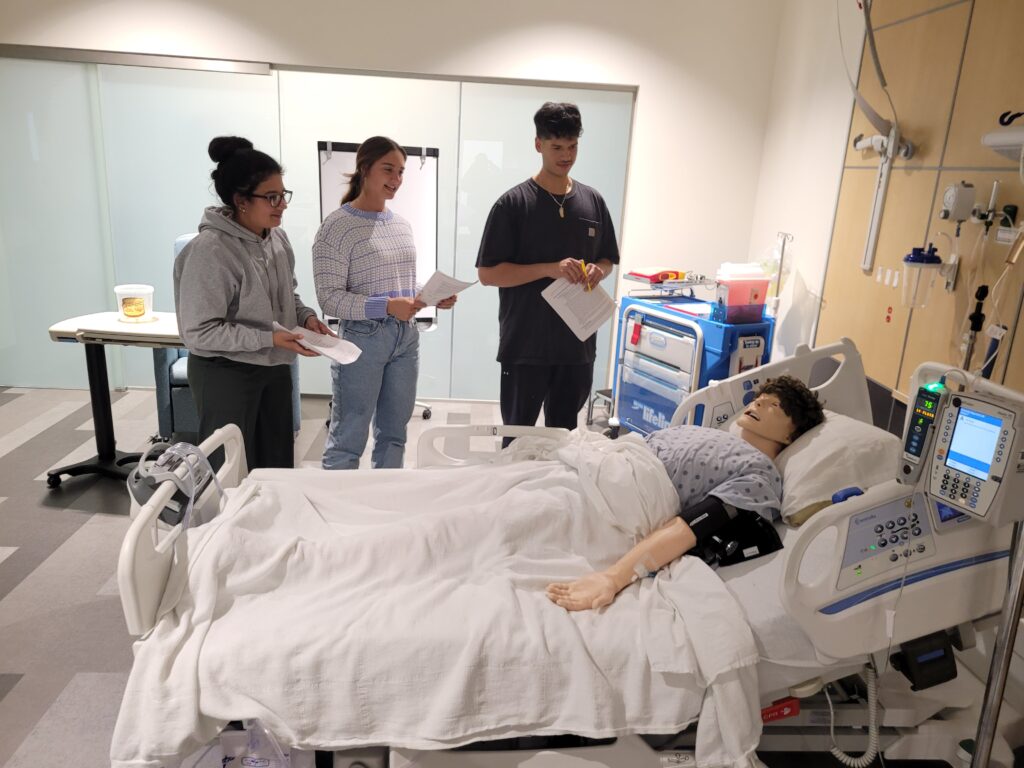
This interprofessional simulation ideally can be worked on in small interprofessional groups, so they can directly work together with the patient. In reality with packed class schedules and busy students, its execution was more akin to a hospital setting, where practitioners see the patient individually, but only access notes in their chart. Classes of students went through at different times, but their case is built upon the information from the other disciplines.
Dr. Tobyas said, “Scheduling can be an issue when creating a simulation, we can’t always get classes to do the simulation in order, such as the patient sees the Nurse, Speech-Language Pathologist, Dietician, and Social Worker. But we can design the case with the ideal conclusions from each discipline, so the students can become familiar with terminology from other disciplines and work together to best treat their patient.”
The initial run of this simulation happened with both Social Work and Dietetics students with great success. In the future it can be expanded or tweaked to include speech-language-pathology, audiology, nursing and even athletic trainers.
Tobyas said, “Simulation is typically thought of as nursing specific avenue of training, but it can be beneficial to multiple disciplines of students who can practice with a manikin, before working with real patients, and that’s important. Learning about how the disciplines work together to treat a patient is also not something most of students experience until they are in professional practice. This is extra preparation they may not get at other institutions.”